The Vagus Nerve, Trauma & Nervous System Healing
Rewiring Safety From the Inside Out
By Astra Sbizzirri – Inner Balance Dynamics
1. Trauma Isn’t Just in the Mind—It’s in the Body
When we think about trauma, we often focus on emotional or psychological symptoms. But the truth is—trauma doesn’t just live in the mind. It lives in the body, particularly in our nervous system. Many people on a healing journey experience a dysregulated nervous system without even realising it. We may find ourselves anxious for no reason, shutting down when overwhelmed, or constantly living in survival mode.

These aren’t character flaws or personal failures. They’re biological responses, and at the center of these responses is a powerful pathway of healing—the vagus nerve.
2. What Is the Vagus Nerve—and Why It Matters for Healing
The vagus nerve is the longest cranial nerve in the body. It connects the brainstem to the lungs, heart, digestive system, and beyond. It plays a crucial role in the parasympathetic nervous system—often called the ‘rest and digest’ system.
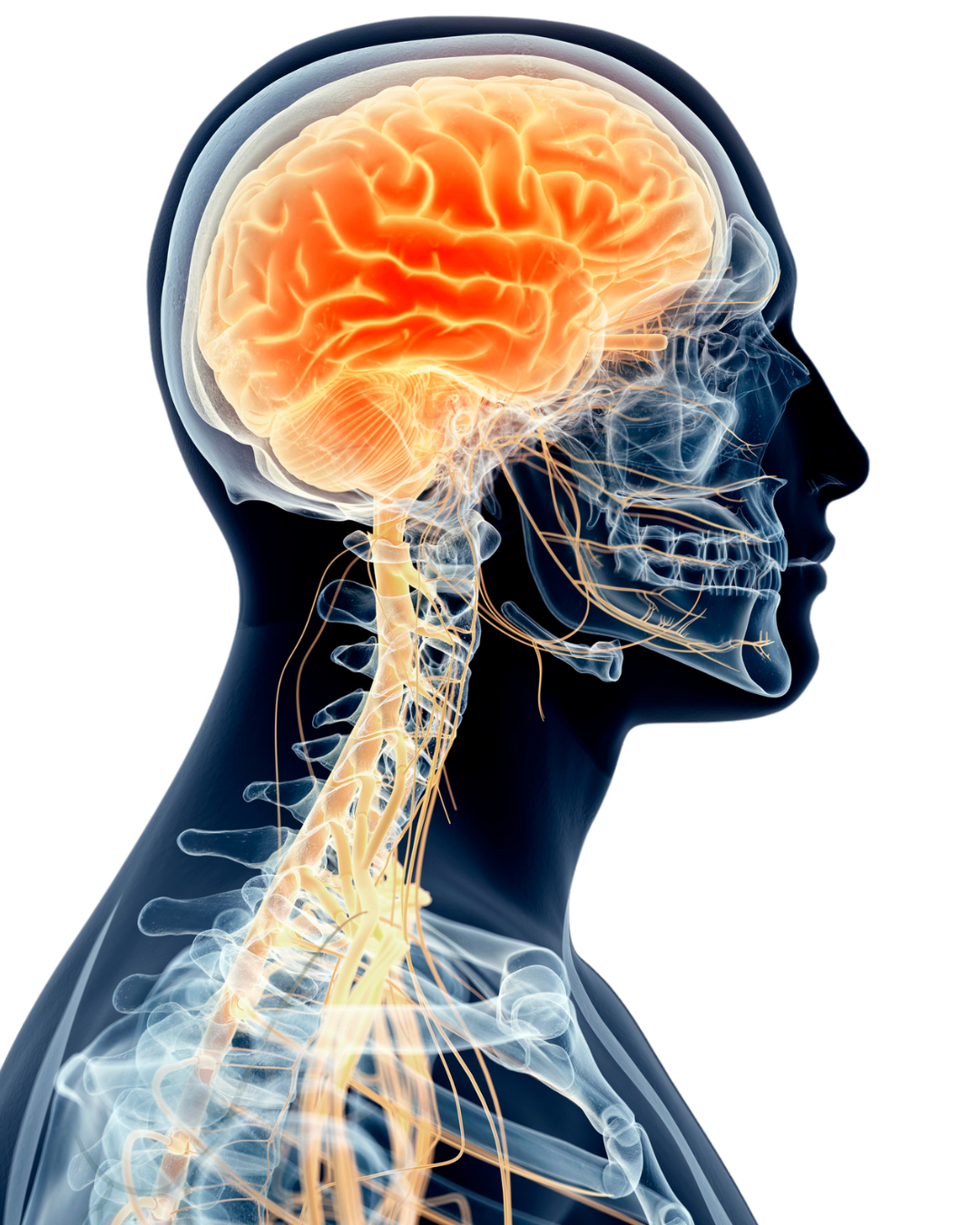
When activated, the vagus nerve helps regulate our heart rate, slow our breathing, support digestion, and calm the mind. It also connects to our ability to feel safe, grounded, and socially connected.
Trauma can disrupt vagus nerve function, leaving the nervous system stuck in patterns of fight, flight, freeze, or fawn. This dysregulation is the body’s attempt to protect us—but it can also prevent us from feeling truly present and well.
3. Signs of a Dysregulated Nervous System

Some of the most common symptoms of a dysregulated vagus nerve include:
– Chronic anxiety or restlessness
– Emotional numbness or disconnection (dissociation)
– Digestive issues
– Difficulty taking deep breaths
– Poor sleep or constant fatigue
– Overwhelm in social settings
Irritable Bowel Syndrome (IBS): Irritable Bowel Syndrome is strongly connected to a dysregulated nervous system and vagus nerve dysfunction—this is well-supported by both clinical research and trauma-informed neuroscience. The vagus nerve is a critical modulator of gastrointestinal function. Stimulating the vagus nerve has been shown to reduce inflammation and normalise gut motility.

Bonaz, B., Sinniger, V., & Pellissier, S. (2016). Vagus nerve stimulation: A new promising therapeutic tool in inflammatory bowel disease and functional gastrointestinal disorders. Frontiers in Neuroscience, 10, 354. https://doi.org/10.3389/fnins.2016.00354
In my own journey, I’ve experienced many of these symptoms without knowing their root cause. Learning about the vagus nerve gave me the language, the tools and awareness to begin healing from the inside out. Learning about the vagus nerve has been a game-changer for me!
4. Rebalancing the Vagus Nerve: 6 Simple, Science-Backed Practices
Healing the nervous system isn’t about forcing change—it’s about creating safety. Here are six gentle practices to stimulate and balance the vagus nerve:

1. Breathwork (especially long exhales): Slow, steady breathing tones the vagus nerve and helps regulate the stress response. Breathwork reduces PTSD, anxiety, and depression
evidence shows that breathing interventions—especially coherent breathing (5–6 breaths/min)—help decrease symptoms of trauma and increase emotional regulation.
Brown, R. P., & Gerbarg, P. L. (2005). Sudarshan Kriya Yogic breathing in the treatment of stress, anxiety, and depression: Part I—neurophysiological model. Journal of Alternative and Complementary Medicine, 11(1), 189–201. https://doi.org/10.1089/acm.2005.11.189
2. Humming, chanting, or singing: Vibrations from your voice stimulate the vagus nerve and invite calm. Singing, chanting, or toning releases oxytocin and reduces cortisol.
Fancourt, D., Aufegger, L., & Williamon, A. (2016). Singing modulates mood, stress, cortisol, cytokine and neuropeptide activity in cancer patients and carers. Frontiers in Psychology, 7, 1189. https://doi.org/10.3389/fpsyg.2016.01189
3. Cold exposure: Splashing cold water on your face or taking a short cold shower can activate the vagus nerve and reset your system. The polyvagal theory by Dr. Stephen Porges also highlights that sensory stimuli (like cold water) can help bring the nervous system into a regulated state by engaging the vagus nerve and increasing vagal tone.
4. Body-based practices (Yoga, Qigong, Tai Chi gentle movement): Movement, especially when mindful, helps the body discharge stress and find balance. Yoga significantly reduces PTSD symptoms in survivors by helping them reconnect with their bodies.
Van der Kolk, B. A., Stone, L., West, J., Rhodes, A., Emerson, D., Suvak, M., & Spinazzola, J. (2014). Yoga as an adjunctive treatment for posttraumatic stress disorder: A randomised controlled trial. Journal of Clinical Psychiatry, 75(6), e559–e565. https://doi.org/10.4088/JCP.13m08561
5. Safe connection: Eye contact, heartfelt conversations, and physical touch can regulate the nervous system through the social engagement system. Human connection—especially when safe, attuned, and non-judgmental—activates the ventral vagal branch of the vagus nerve.

This system:
- Regulates heart rate, breath, and facial expression
- Supports emotional co-regulation
- Signals to the brain and body that it is safe to relax
- Is biologically wired into us for survival, bonding, and healing
- If we don’t experience safe connections in our childhood, this negative experience deeply affects our entire nervous system with a lasting impact into adulthood.
- Positive social interactions enhance vagal tone, reduce cortisol, and improve heart rate variability.
Feldman, R. (2007). Parent–infant synchrony and the development of shared timing and intention. Developmental Psychology, 43(2), 329–343. https://doi.org/10.1037/0012-1649.43.2.329
6. Limit caffeine/stimulants, especially if you are physically sensitive: stimulants can cause a state of dysregulation of the nervous system. Caffeine is a central nervous system stimulant. It increases adrenaline and cortisol, which activate the sympathetic “fight or flight” response. While this can enhance alertness short-term, for people with trauma histories or existing dysregulation, it can:
- Increase anxiety
- Aggravate panic symptoms
- Cause sleep disruption
- Heighten heart rate or jitteriness

🔬 Research shows that caffeine increases noradrenaline and cortisol secretion, particularly in those under chronic stress or with PTSD. This can exacerbate dysregulation in people who already struggle with nervous system balance.
Childs, E., & de Wit, H. (2006). Subjective, behavioural, and physiological effects of acute caffeine in light, nondependent caffeine users. Psychopharmacology, 185(4), 514–523. https://doi.org/10.1007/s00213-006-0341-3
5. Final Thoughts: Healing Is Nervous System Work
What I have learned through my studies of anatomy & physiology, biochemistry, energy healing, and trauma recovery coaching, trauma recovery isn’t just about mindset—it’s also about biology, biochemistry and the nervous system. When we work with the vagus nerve, we work with the body’s blueprint for safety and connection. When we are aware of the vagus nerve and its role in the body, we can switch off the “fight or flight” survival response to feeling connected and safe in our bodies and our environment.

The more we support our nervous system, the more we reclaim our sense of peace, presence, and empowerment. Healing is possible—and it begins within, with inner balance!
